Research design, sample and setting
The study used a double-blinded, randomized controlled trial with a two-group pretest–posttest design; the older adults and outcome evaluators (research assistants) were blinded. The population of interest was community-dwelling older adults living in a semi-urban community in central, northeastern Thailand. We applied multi-stage sampling for this study, starting with cluster sampling, followed by simple random sampling. The cluster sampling was used to select two similar semi-urban communities from 18 communities. The two communities are about 12 km from downtown and super tertiary hospitals, providing call centers, ambulances, emergency services, and advanced cardiac procedures. These two semi-urban communities also had primary care units, and people living there had similar lifestyles and occupations. After study settings randomization was done, a simple random sampling was used to include older adults in each group; this was done by drawing lots (house numbers) from all meeting inclusion criteria from the two communities. The sample size was determined using the equation for experimental research that compares means between two independent groups35 and based exclusively on a previous study by Sanprakhon, Choosri, and Wongviseskul30. With an alpha level of 0.05, a power of 0.95, a variance of 3.12, and a mean difference of 2.23, a power analysis determined that 43 participants would be necessary for each group. However, the 10% possible dropout rate was added for sample size calculation, and 48 older adults for each group would be enough, meaning 96 community-dwelling older adults participated in this study.
Inclusion and exclusion criteria
Eligibility to participate in the study was based on seven criteria: (1) male or female between the ages of 60 and 80 years old; (2) capable of reading and writing Thai; (3) oriented to time and place; (4) no hearing and visual problem; (5) no depression symptom as screening with a 2-question (2Q) depression screening form (Respond “No” for both questions), or dementia as screening with the Thai Mental State Examination (score ≥ 23 points); (6) no disturbing signs/symptoms, such as knee osteoarthritis, severe pain (10-point numerical scale ≥ 5 points) or high fever (axillary temperature ≥ 38.5 °C) to join program activities such as role-play and Emergency Call (1669) situation; and (7) willing to participate in this study by completing consent form. In cases of family members or caregivers of older adults who are required to participate in primary cardiopulmonary resuscitation (CPR), they must not have any health problems or symptoms that limit the practice of CPR, such as heart disease, chest pain, asthma, or chronic obstructive pulmonary disease (COPD), arthritis, severe pain (PS ≥ 5 points), high fever (BT ≥ 38.5 degrees), or abnormal vital signs.
Exclusion criteria were (1) older adults with an acute illness after starting the activity, such as low blood pressure, difficulty breathing, chest pain, and dizziness, and (2) Older adults participating in less than 6 out of 8 activities.
Data collection
The total number of older adults in the two communities was 674; however, 142 did not meet the inclusion criteria, and 31 declined to participate. Only 501 were randomly included in this study using simple random sampling (drawing lots of house numbers). Finally, the 96 participants were randomly included in the control or experimental groups. These two groups lived in different sites and were about 12 km away from downtown, and they did not know they were in control or experimental groups. Moreover, the two research assistants were allowed to participate in this study only for outcomes evaluation, and they did not know they were measuring outcomes for participants in control or experiential groups. The two research assistants not working in these two communities assessed their knowledge, beliefs, and decision-making a week before starting this study. They re-evaluated these outcomes a week after finishing the intervention. The experimental group received a health education applying role-play promoting decision-making ability program and home visits for eight weeks to improve their knowledge, belief, and decision-making, and the control group received routine care, home visits, and brochures during the same period. The study lasted from November 2021 to April 2022.
Research instruments
-
1.
Screening: The depression symptom was screened using a 2-question (2Q) depression screening form with a sensitivity of 97.3 and a specificity of 45.636. Cognitive function was screened using the Thai Mental State Examination (TMMSE) with a sensitivity of 82 and a specificity of 7037. The TMMSE also achieved Cronbach’s alphas as 0.8138.
-
2.
Demographic and clinical information: This included sex, age, marital status, education level, income, occupation, health insurance, health status, chronic diseases, self-experience of AMI, and seeing or knowing other persons experiencing AMI.
-
3.
Primary outcomes: Knowledge was measured by the 12-item knowledge of coronary artery disease (CAD) risk factors and the 15-item knowledge of AMI symptoms. These two questionnaires had three response items, including “yes”, “no,” and “not sure.” If older adults checked “yes” for the correct answer, they got one score, but if they checked “no” for the correct answer, they got zero. Older adults who checked “not sure” got zero for every question. The total scores were 12 and 15, respectively, and the test–retest reliability for these two questionnaires was 0.78 and 0.90, respectively13.
The belief was measured by six questionnaires, including the four items of perceived susceptibility, 15 items of perceived severity, four items of perceived benefit, 15 items of perceived barrier, four items of perceived self-regulation, and four items of perceived cue to action. There were six response items for perceived susceptibility and cue to action from 1 (not at all) to 6 (very likely), and six response items for the other four questionnaires for 1 (strongly disagree)–6 (strongly agree). Total scores for each questionnaire were 24, 90, 24, 90, 24, and 24, and Cronbach’s Alpha Coefficients were 0.90, 0.95, 0.92, 0.90, 0.90, and 0.84, respectively13,39.
The two questions measured decision-making; one asked how likely the older adults were to take seven of any actions (such as calling emergency service/1669, taking medicine, drinking water, and smelling cologne/herb) if they were in the presence of someone having an AMI. This question had seven response items from 1 (not at all) to 7 (certain). We picked only one action, calling 1669, for our analysis, and the other six actions just be provided to not guide the best action for older adults for the next question. The second question asked older adults to choose the best first plan-of-act when they were in the presence of someone having an AMI. This question had seven choices, including seven of the above actions. If older adults checked on calling 1669, one was entered; if they checked on other actions, zero was entered for data analysis. Cronbach’s Alpha Coefficient for this questionnaire was 0.9539. When analyzing data, we prepared the first question as a continuing variable and the second as a dichotomous one.
Intervention
Based on a systematic review, the researchers developed a health education applying role-play promoting decision-making ability program for community-dwelling older adults28. The structure of this program was a health belief model, the details were based on systematic review results, and the content was updated with the content suggested by the American Heart Association. The program content included heart disease and AMI, etiology, signs and symptoms, treatment and management, emergency service and call, appropriate action in AMI situations, cardiopulmonary resuscitation (CPR) training, appropriate decision-making activities, asking for help, and program review. Moreover, role-playing related to each activity was used to draw attention from the older adults before starting the program.
This program was proved by five experts, including two cardiologists, two cardiac nurses, and one researcher who was an expert in gerontological nursing. The program’s activities and materials relied on the principle of providing health education concerning aging processes and impairment40,41,42. We spend a short period and divide health education programs into a few short sections. Teaching strategies included both class teaching (lecture) and practicing. The tasks for practicing were uncomplicated, including a few steps, and they were done step by step. Health educators provided a good environment and appropriate places for teaching and training. The teaching style considered the context and culture of older adults. Suitable media were applied to communicate health information to this target group, as well as large letters and visible pictures to read and see.
Moreover, uncomplicated sentences, informal language, and friendly colors were provided. Finally, a handbook was provided for older adults to take back home to review. This program included eight-week activities, which each week started with a greeting and introduction (5 min), role-playing about the situation related to weekly activities (10 min), giving health education/training health activities (15–30 min), and conclusion (5 min). There were between 45 and 60 min in total for each session. Finally, the handbook was prepared using large letters, black letters on a yellow background, simple and informal sentences, clear pictures, and brief content/short text. Before conducting this research, this program was piloted with ten older adults to ensure its feasibility and acceptability. This program was able to draw attention from and suitable for older adults; however, two unclear pictures were suggested to be changed, and the size of the letters was suggested to make it bigger from 18 to 20. Then, it was revised based on the limitations and suggestions of older adults. The final eight-week activities with all details are shown in the figure (Fig. 1).
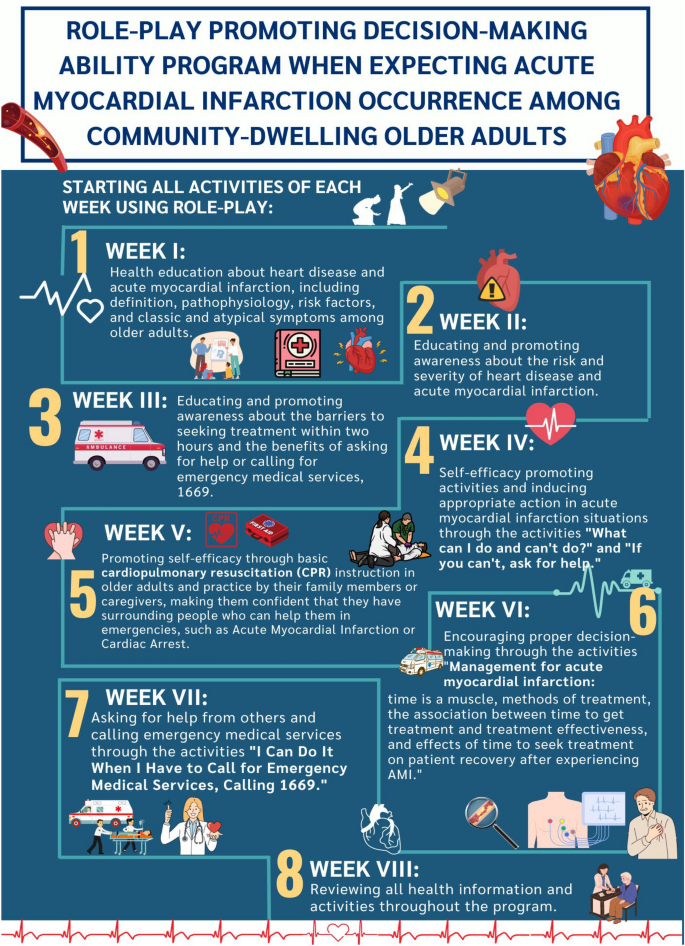
Health education applying role-play promoting decision-making ability program.
In the control group, the participants received brochures and home visits by the registered nurses in their community setting. The participants had chances to ask questions and discuss when measuring vital signs during home visits. This home visit was once a week with or without the participant’s family members.
Validity and reliability
The study protocol was developed and prospectively registered to avoid bias, and this study was conducted strictly following the registered protocol. A checklist for all activities was provided and completed to confirm that the primary investigator did all activities and procedures following the protocol. To avoid bias, a randomized was performed two times, including cluster sampling and simple random sampling, and a double-blinded design was applied (research assistants and participants did not know which groups were control or intervention groups). The four actors who performed role-play earned a bachelor’s degree in nursing. They were trained and performed acting rehearsals many times until they achieved this program’s main points of health information and aims before performing role-play to older adults. Moreover, the two research assistants participated in the recruitment and data collection processes (baseline and post-intervention). However, the principal researcher only implemented intervention using a flipchart and PowerPoint. The two research assistants earned master’s degrees in nursing, had research experience, and were trained for screening and data collecting before starting this study. All questionnaires were checked twice and completed before the older adults left the school. The screening process and findings were reported using the diagram and standard statement.
Ethical considerations
The research received approval from the Khon Kaen University Center for Ethics in Human Research (Approval Number: HE642163) on July 15, 2021, following the ethical principles of the Declaration of Helsinki. Volunteers who participated in the study received information about the purpose of the research, confidentiality of data, reporting data in the aggregate, and the ability to withdraw from the study without losing care or medical treatment—those who agreed to participate signed informed consent. Finally, the study protocol was prospectively registered on 28/09/2021, and the clinical trial registration number was TCTR20210928004.
Data analysis
Data were analyzed initially by calculating descriptive statistics using the IBM® SPSS® version 28 statistical software under a university license. Demographic characteristics between control and experimental groups were compared by applying the Chi-square Test, Fisher Exact Test, and Independent t-test. Normal distribution was explored using Kolmogorov–Smirnov and Shapiro–Wilk, Skewness and Kurtosis, Histogram, and normal Q–Q and Box plots before exploring between-groups and within-group comparisons. In normal distributions, independent-sample t-tests were examined for knowledge, belief, and decision-making differences between the experimental and control groups. However, the Mann–Whitney U test was applied for non-normal distribution variables.
In the same way, in cases of normal distribution, paired-sample t-tests compared within-group differences; however, the Wilcoxon (Matched Paired) Signed Rank test was applied for non-normal distribution variables. A Chi-square was generated when comparing a categorical variable, first of action. Finally, the adjusted analysis was performed to explore actual results after we found that sex, income, and knowledge of risk factors differed between control and experimental groups at the baseline.
link

